|
Affiliated to: |
|
 |
||||||||||||
ICD/CRT Patient Info |
||||||||||||
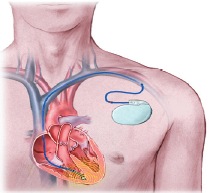
What is an Implantable Cardioverter Defibrillator (ICD)?ICD stands for Implantable Cardioverter Defibrillator. It is made up of a small, slim, box shaped device which contains a battery and electronic circuits. The device is connected to your heart by wires known as leads. The leads are passed along a blood vessel to your heart and the ICD box is usually implanted under the skin in your upper chest, near your collar bone. The ICD can recognise and monitor your heart rhythm and can give you some treatments if needed. It also stores information about your heart rate and rhythm which can be accessed when you come to the clinic for follow-up What is Cardiac Resynchronisation Therapy?Cardiac Resynchronisation Therapy (CRT) devices are used to help to treat heart failure and can be either a permanent pacemaker or an ICD. They work by making the heart chambers pump at the same time (synchronously) and improve the overall function of the heart so that you feel lees breathless and have more energy. What can the ICD do?Most modern ICDs have three main functions; however you may not need to have all of them. Your Cardiologist will select what settings are best for your condition.
What can CRT do?There are 2 different types of CRT devices:
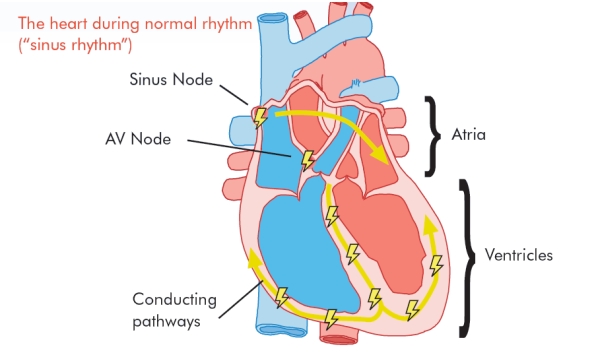
CRT PacemakersThese devices work in the same way as traditional pacemakers. They help the heart to beat in a regular rhythm and are especially useful when the heart’s natural pacemaker stops working properly. An implanted pacemaker sends out electrical signals which make the heart beat in a normal way. A The main pumping chamber of the heart is on the left side, called the left ventricle. In a normal heart, both the right and left ventricles pump out blood at the same time in a coordinated way. In heart failure, the left side may not pump at the same time as the right, meaning the two sides of the heart lose their coordination. This leads to the heart being unable to pump effectively and you may become breathless, dizzy and have no energy. Over time, the heart may get even weaker and you may feel more unwell. In this case, your doctor may feel that you could benefit from having a CRT pacemaker implanted. The main difference is that an additional lead is placed on the left side of the heart and electrical signals can make the left ventricle beat at the same time as the right. This can restore the heart’s coordination and make the heart pump more efficiently. In two out of three people implanted with a CRT pacemaker, symptoms of breathlessness improve and they have more energy and generally feel more healthy. CRT ICDsYou may have had a dangerous rhythm problem in the past known as ventricular tachycardia (VT) or ventricular fibrillation (VF). These happen when an electrical problem causes the heart to beat too fast and may lead to the heart being unable to pump blood around the body, causing a cardiac arrest. If not treated with an electric shock, death can occur in a few minutes. You may not have had a dangerous rhythm before, but you may be at risk of having one in the future because of your underlying heart condition. In this case your doctor may recommend that you are fitted with an ICD instead of a pacemaker. Having an ICD means that if you ever need an electric shock because your heart rhythm has become dangerously fast, it will be delivered within seconds. However, you may not always need a shock to return your heart rhythm to normal. Quite often extra signals from the pacemaker part of the ICD can make the heart rhythm normal again. This is known as anti-tachycardia pacing (ATP) and works about 85% of the time to treat ventricular tachycardia. A standard ICD is fitted like a normal pacemaker, with either one or two leads in the right side of the heart. A CRT ICD has the extra lead on the left ventricle which makes the heart pump in a coordinated way, improving symptoms of heart failure. Why do I need one?Your Cardiologist will advise you. However if the doctor has suggested that you need a defibrillator you may have experienced OR will be at risk of experiencing an abnormal, fast heart rhythm that can cause you to become unwell, unconscious, or your heart to stop beating. How the heart works normallyThe heart is a muscle, its function is to pump blood and oxygen around you body to all of your vital organs. It has four chambers, two at the top (the right and left atrium) and two at the bottom (the right and left ventricles). The heart also has an electrical system, which sends impulses (beats), through the heart causing it to contract and pump blood around the body. Each normal heartbeat begins in the natural pacemaker of the heart (the sino-atrial or SA node) which lies at the top of the right atrium. It then travels across the two top chambers and down through a small junction box (the atrio-ventricular or AV node) which lies between the upper and lower chambers. It then spreads across the bottom chambers causing the heart to contract and pump. |
||||||||||||
 |
||||||||||||
|
Sometimes the electrical system in your heart does not work as well as it should. This can cause your heart to beat too quickly. The defibrillator can stop fast heart rhythms that start in the ventricles, the bottom two chambers of the heart. This fast heart rhythm is called ventricular tachycardia or VT. This can sometimes start after a heart attack or in people who have angina. There are several other reasons that you may benefit from having an ICD, even if you have never had an abnormal heart rhythm. You may have a heart condition that puts you are at risk of having an abnormal rhythm in the future. Your Cardiologist will explain these reasons to you. Some people can have an even faster, irregular heart rhythm called ventricular fibrillation or VF. This is life threatening if it is not treated quickly with an electric shock delivered to the heart. You may need to have some tests before the decision to have an ICD fitted is made. Your Cardiologist will advise you if these are needed. Who needs a CRT device?These devices do not work for all types of heart failure and you may need to have a heart scan (echocardiogram) to check the pumping function of your heart. It is also important to note that any device is not a replacement for your heart failure medication. Why might I need a CRT Pacemaker?
Why might I need a CRT ICD?
How is the defibrillator implanted?Your Cardiologist will have explained to you why you need to have an ICD and the benefits from having an ICD fitted. You need to know how having a defibrillator fitted will affect you as well as what could happen to you if you do not have one fitted. This will all be explained to you and if you agree to go ahead, you will be asked to sign a consent form. You will also be given a booklet explaining the consent form before you sign. Your ward nurse and a porter will take you to the cardiac pacing theatre or catheter lab. Once you are in the pacing theatre, another nurse will check your details again and you will be asked to lie on a trolley or narrow operating table. The procedure is not usually performed under a general anaesthetic, but you will be given sedation, which will make you relaxed and sleepy. Before the procedure starts, the doctor will inject some local anaesthetic under the skin just below your collarbone (usually the left side). This will numb the area and allow the doctor to pass a small lead or electrode through a vein into your heart. You may have two or three leads inserted depending on what your doctor recommends. The leads are then connected to the pulse generator box, which is about the size of a small matchbox. This will be placed under the skin in your chest. The doctor will test the device during the procedure. This will make your heart beat very quickly and the defibrillator will give a shock to make sure the ICD works properly. You will be given some sedation before this happens, so you should not feel the shock. The area will then be stitched with dissolvable or non-dissolvable stitches. If your stitches need to be removed by your GP, Practice Nurse or District Nurse you will be informed before you leave hospital. |
||||||||||||
 |
||||||||||||
What happens after the ICD is fitted?After the procedure and once all the checks have been made, you will be taken back to the Cardiology ward. You will be asked to lie in bed for a couple of hours then you can get up and eat and drink. As the wound can feel quite bruised and sore, especially for the first day or two, your nurse will give you regular painkillers. It is very important that you tell your nurse immediately if you have any pain at all. You will also be given some antibiotics to take before and after the procedure to minimise the risk of infection. The wound should be kept clean and dry until it has fully healed, although it is fine to have a bath or shower after the rest three or four days. Ask your nurse for a protective dressing so that you can bathe without wetting the wound. Report any wound problems to your nurse. You should not lift the arm on the same side as the defibrillator (usually the left arm) above shoulder level until you have been for your first follow-up appointment, normally 4-6 weeks later. This is because there is a small chance that the leads can move out of position. However it is important to do gentle arm and shoulder exercises to keep the arm mobile. You should avoid any vigorous or violent movement of that arm until you have had your first ICD check-up. Your Cardiologist will visit you on the ward at the end of the day and you will probably be allowed to go home the next day provided your ICD is checked, there are no complications and your doctor assesses it is safe. Your ICD will be checked before you go home by a Cardiac Physiologist or the ICD Nurse Specialist. This check will involve the use of a special programmer that can look at the device settings and make sure the ICD is working properly. This check takes about 15 minutes and can either be done on the ward or in the Outpatients’ department. After this check most patients will also have a chest x-ray to check lead positions and make sure all is well following the implant procedure. Please ask the physiologist or ICD nurse if you have any questions or worries about the device. You will be given an ICD identity card, emergency information, and instructions at this check, and also a helpline number should you have any queries. Going homeAlthough most people feel very pleased to be going home, it is only natural that you may feel a bit worried. This is very common, especially if you have been in hospital for a long time and the ICD has only just been put in. However, we try to make sure that you get the help you need to return to as full and active a life as possible. Please feel free to ask questions at any time. Similarly if you feel upset or ‘down’ once you are at home it is very important that you talk to someone. Please contact your ICD implanting hospital if you have any concerns. Arm movements - Extra tissue will grow around the lead(s) in your heart after a few weeks, which will prevent the wire(s) moving out of place. Try to avoid lifting the arm on the same side as the ICD above shoulder level until you have had your first outpatient check. Please contact your ICD implanting hospital if you have any concerns. Arm movements - Extra tissue will grow around the lead(s) in your heart after a few weeks, which will prevent the wire(s) moving out of place. Try to avoid lifting the arm on the same side as the ICD above shoulder level until you have had your first outpatient check. Wound site - Your wound site should take about six weeks to fully heal. Try to avoid wearing tight clothing over the wound until it has healed completely to avoid excess rubbing over the area. If you notice any redness, soreness or swelling of the area, or any signs of bleeding or oozing from the wound, report this immediately to your GP as these may be a sign of wound infection. You will probably be able to feel the defibrillator box under your skin as well as other lumps close by. These are the leads that are attached to the box, curled up beside the box under the skin. It is extremely important that you don’t try to move the box or leads, but please let someone know if they continue to bother you. Will I feel the treatment from the ICD?The device will be programmed to the best settings for you. Your Cardiologist will do this initially when the ICD is implanted, but settings can be modified during your follow up appointments in the clinic if necessary. The ICD can give the following treatments, but you may not have all of them programmed if you do not require them. Your physiologist or ICD nurse will be able to tell you what your device has been set to do. Anti-bradycardia pacing pulsesIf your heart is beating too slowly, the ICD can send small impulses through the heart which generate extra heart beats when required. As these impulses are very small they are not painful and are not usually noticed. Also, sometimes the heart can beat slowly for a few seconds following treatment for a fast heart rhythm. The device can tell when extra beats are needed and give extra beats as necessary. Anti-tachycardia pacing pulses (ATP)If your heart beats too fast, the device can send out faster pacing impulses which can help to get the heart back into a normal rhythm. This can be done so quickly by the ICD that many people do not know that this has even happened. Sometimes it can make you aware of having palpitations or of feeling dizzy. If the ATP does not correct your fast heart rhythm your device will be able to deliver a shock. Cardioversion shocksYour ICD may be programmed to give shocks to your heart on a specific part of the heartbeat. This type of shock is used to treat ventricular tachycardia. The energy used in this shock may be the same or less than is used in a defibrillation shock and you may still find this quite painful. Your ICD may be programmed to give a few small shocks to your heart if it recognises that your heart is beating too quickly. The energy used in the shock is much smaller than is used in a defibrillation shock, you may still find this a little painful but it will pass quickly. Defibrillation shocksThese are larger energy shocks which the device will deliver if it senses that your heart is beating so fast that it is life-threatening These fast heart rhythms are called ventricular tachycardia and ventricular fibrillation. Patients have reported that this feels like they have been suddenly kicked or punched in the chest. These shocks can be quite painful but the pain will only last for a few seconds. Some people may not feel anything if their heart is beating so fast that they have become unconscious. If someone is with you when you have the shock, they will probably notice you jolt. No harm will come to anyone who is touching the patient when they receive a shock. Indeed, it can be very comforting and reassuring to have someone put their arm around you as you experience a shock. When you come to the ICD clinic your physiologist or ICD nurse will examine your device and any treatments will be detected. What should I do if the ICD gives me a shock?You may have some warning that your ICD is about to deliver a shock such as feeling palpitations, or feeling light-headed or dizzy and be able to take the following safety steps. However this may happen so quickly that you have no warning at all. If you do think that you are about to receive a shock, you should sit or lie down on the ground. You should also let someone know how you are feeling if possible. Afterwards you should recover quite quickly. Even if you feel well after the shock you should still contact the implant centre as son as you can to arrange to have your device checked. You may need to leave a message on the answering machine, but your call will be returned as soon as possible. After a while, it is not necessary to have the device checked following each shock unless you feel unwell. However, if you feel unwell or if your device has given you several shocks please dial 999 for an ambulance to bring you into your nearest hospital. Your ICD will be checked to fund out why the shock was given. It is extremely important to keep your ICD card with you at all times so that the make, model and settings of the device can be known straight away. Getting back to normalHaving an ICD implanted can be seen as a rather big event in your life. However with help and support most people can adapt well over time. After a fairly short recovery period you should be able to return to previous activities however some restrictions will apply for your own safety. Driving - The Driving and Vehicle Licensing Agency (DVLA) have strict guidelines in relation to patients who require an ICD and whether or not they are safe to drive. There will be some restrictions but these will vary depending on why you have had your ICD fitted. It is very important that you discuss this with your nurse, physiologist or doctor at your ICD centre who will explain this in more detail. You can access the DVLA guidelines on; www.dvla.gov.uk/drivers/dmed1.htm You will also need to tell your insurance company to let them know that you have had an ICD fitted. Physical activity - A certain level of exercise is needed to keep your heart healthy. It is natural to be concerned about the possibility of the ICD delivering a shock or stressing the heart. Following your initial recovery, normally about 4-6 weeks, it is recommended that you try to increase your level of activity if possible. You may be offered cardiac rehabilitation or exercise testing to restore your confidence and get you back to normal. Once your wound has fully healed, you will be able to go swimming if you wish. However you are advised not to swim alone in a private pool or in the sea beside a deserted beach. Contact sports such rugby are not advised as the device or leads can become dislodged. Please talk to the doctors, nurses or physiologists at your ICD clinic if you have concerns about physical activity. Sexual activity - It is very common to be reluctant to resume sexual activity. However the device will not cause any harm to your partner, even if a shock is delivered to you during intercourse. DIY - You can safely use equipment such as electric drills as long as they are in good working order, although you should keep them away from your ICD site. Electromagnetic Interference - Electromagnetic interference will not damage your ICD but will stop it from delivering any treatment for the period of time that you are in contact with it. Most mechanical and electrical devices that you use in your normal daily activities will not affect your ICD. Ordinary radios, fridges, cookers, computers and microwaves will not affect your ICD as long as they are in good working order. In case you ever feel dizzy or experience palpitations whilst using an electrical appliance, you should move away from the appliance and phone the physiologist, ICD nurse or doctor at the ICD clinic for advice. Magnets - Do not carry magnets or place a magnet over your chest. Avoid carrying stereo or hi-fi speakers as they contain strong magnets that can interfere with your ICD. ICD therapies may be temporarily disabled by magnets and in some cases this may be necessary if you received inappropriate shocks from the ICD. Some hospitals give their ICD patients magnets and full instructions on their use. Shop doorway security systems - There is a very small risk of interference to your ICD, so you are advised to walk through shop doorways at a normal pace and not to wait around in this area. Electronic ignition systems - Avoid leaning over the alternator in a car whilst the engine is running, otherwise it is generally safe to work as a mechanic. Medical equipment/other hospital treatments - Most equipment used by your hospital or GP surgery will not cause any problems to your ICD. However it is advised that you let medical and dental staff know that you have an ICD as technical support may be required before some treatments. Please take your ID card with you whenever you go to hospital. It may also be useful to contact your implanting centre for advice before you go into hospital for any investigations or operations that are not associated with your ICD. It is safe for you to have X-rays, CT scans and mammograms. However you should avoid magnetic resonance imaging (MRI) machines. Some electrical nerve and muscle stimulators (TENS units) may cause interference with ICDs but this depends on where they are being applied, and, if this form of treatment is suggested to you then your ICD clinic should be contacted for advice. Travel - You can safely travel abroad with your ICD, but you are advised to show the security staff your identification card and ask to be searched by hand. This is because the hand held wands can temporarily interfere with your defibrillator. Walk through the metal detector archway if asked to do so, but the metal casing of the device may set off the airport security alarm. The detector will not cause any harm to your ICD provided you walk briskly through the arch. You will need to make sure that your travel insurance company is aware that you have an ICD. Some insurance companies require written confirmation from your Cardiologist that you are fit to travel. Travel companies may also try to increase your insurance premiums to outrageous levels and it is suggested that you shop around if this happens. Many ICD clinics carry a list of ICD friendly insurance companies. If you wish, you may be given addresses of defibrillator clinics in the area that you are visiting. Please contact the ICD clinic at least 6 weeks before you intend to travel or check the manufacturer’s website for information. Please be aware that your doctor may advise against you visiting very isolated or remote destinations. Arc welding - This should be avoided but can be performed under special circumstances. Please ask your ICD centre if you need further information on arc welding. Mobile phones - Some studies have shown that mobile phones can affect the ICD if held within 6 inches of the device. It is therefore recommended that you do not keep a mobile phone in a coat or shirt pocket over the ICD. Keep the handset more than 6 inches away from the ICD; ideally hold the phone over the ear on the opposite side to the device. Avoid direct contact with the antenna whilst making or receiving a call. ICD Clinic VisitsYour ICD should be checked regularly and visits may be necessary more often just after the ICD is fitted. During each clinic visit, the physiologist or ICD nurse will examine your ICD using a special programmer. This machine allows us to examine the settings and the battery life of your device. All the information is stored on a computer disc and stored in your records. Your wound will also be checked and you may have other tests done. Please also take this opportunity to ask any questions or let us know if you have any problems or worries. You may also see the cardiologist or their registrar at your clinic visit. Changing the defibrillatorNormally an ICD battery lasts between four and seven years. Your battery will be checked at every visit to the ICD clinic and staff at the clinic will be able to predict when you need a new ICD box. It will not be allowed to completely run down. In order to have the box changed, you will need to be admitted to hospital. The procedure is similar to having your first ICD fitted, but it will not usually involve having new leads put in. Unfortunately you will be restricted from driving for a week after the new box has been put in, unless there have been any other problems. Clinic staff will be able to advise you on your individual case. Contacting the ICD ClinicMost ICD clinics/support services run between 9am and 5pm Monday to Friday. Ask staff at your implant centre about arrangements to contact them outside these hours. |
||||||||||||
